CORMAC x Health Datapalooza 2022: The Intersection of Nursing Homes, COVID-19, and Social Determinants of Health
 At the 2022 Health Datapalooza and National Health Policy Conference, CORMAC’s Health Analytics Lead, Dr. Pam Phojanakong presented research that analyzed how Social Determinants of Health (SDOH) played out at Nursing Homes during the height of the COVID-19 pandemic. CORMAC is no stranger to Nursing Home data: we’ve successfully partnered with CMS/CCSQ/Division of Community Post-Acute Care (DCPAC) since 2015 across two distinct projects to drive better outcomes for some of the nation’s most vulnerable populations.
At the 2022 Health Datapalooza and National Health Policy Conference, CORMAC’s Health Analytics Lead, Dr. Pam Phojanakong presented research that analyzed how Social Determinants of Health (SDOH) played out at Nursing Homes during the height of the COVID-19 pandemic. CORMAC is no stranger to Nursing Home data: we’ve successfully partnered with CMS/CCSQ/Division of Community Post-Acute Care (DCPAC) since 2015 across two distinct projects to drive better outcomes for some of the nation’s most vulnerable populations.
Background: More than 40% of COVID-19 deaths in the US from October 2020 to February 2022 were in Nursing Homes even though Nursing Homes only accounted for 8% of all cases. Despite this, Nursing Home Staff have been reluctant to receive the vaccine. According to the December 2020 National Association of Health Care Assistants survey, the majority of Nursing Home staff did not plan on getting vaccinated and only 44.3% had the booster. To track and address this issue, the Centers for Medicare and Medicaid Services (CMS) established vaccination reporting requirements for Nursing Home Staff members and residents in May 2021. However, because CMS did not require Nursing Homes to report race/ethnicity data for COVID-19 cases and deaths, the full impact of COVID-19 and any disparities in vaccination rates remains unclear.
A Place-Based Approach: Given the disproportionate impact of COVID-19 on both nursing homes and on communities of color, we used a place-based approach to examine the role of SDOH in vaccination rate variation among Nursing Homes early in the pandemic. Using facility-level geographic information from the May 30, 2021 CMS COVID-19 Nursing Home data, county-level health metrics, socioeconomic, and race/ethnicity data were linked to information on COVID-19 deaths, case counts, vaccination rates, along with medical supply availability, staff counts, and occupancy rates for Nursing Homes. County-level data was taken from 2021 County Health Rankings, a compilation of data from the American Community Survey, the Behavioral Risk Factor Surveillance System, National Center for Health Statistics, and Mapping Medicare Disparities Tool.

Analysis: Through geographic linking, we were able to link SDOH data to 6,695 Urban and 2,098 Rural Nursing Homes. With more than 200 variables to examine, Principal Components Analysis (PCA), a dimensionality reduction method used in machine learning was used to transform these many, potentially correlated variables into a smaller and more coherent set of uncorrelated factors (principal components or PCs). Using PCA, we found that SDOH accounted for the largest share of variance. However, the driving factors were different between urban and rural Nursing Homes.
Overall, 5 PCs accounted for 44.2% of the variation in Urban Nursing Homes and 37.7% of variation in Rural Nursing Homes. Below, we present two of the five PCs with the most significance. Urban Nursing Homes are driven by low English proficiency, overcrowding, unaffordable housing, and proportion of White and Hispanic residents in the county contributed to 14% of the variance among urban Nursing Homes. For rural Nursing Homes, county food insecurity, poor health, low educational levels, and broadband access contributed to 13% of the variance.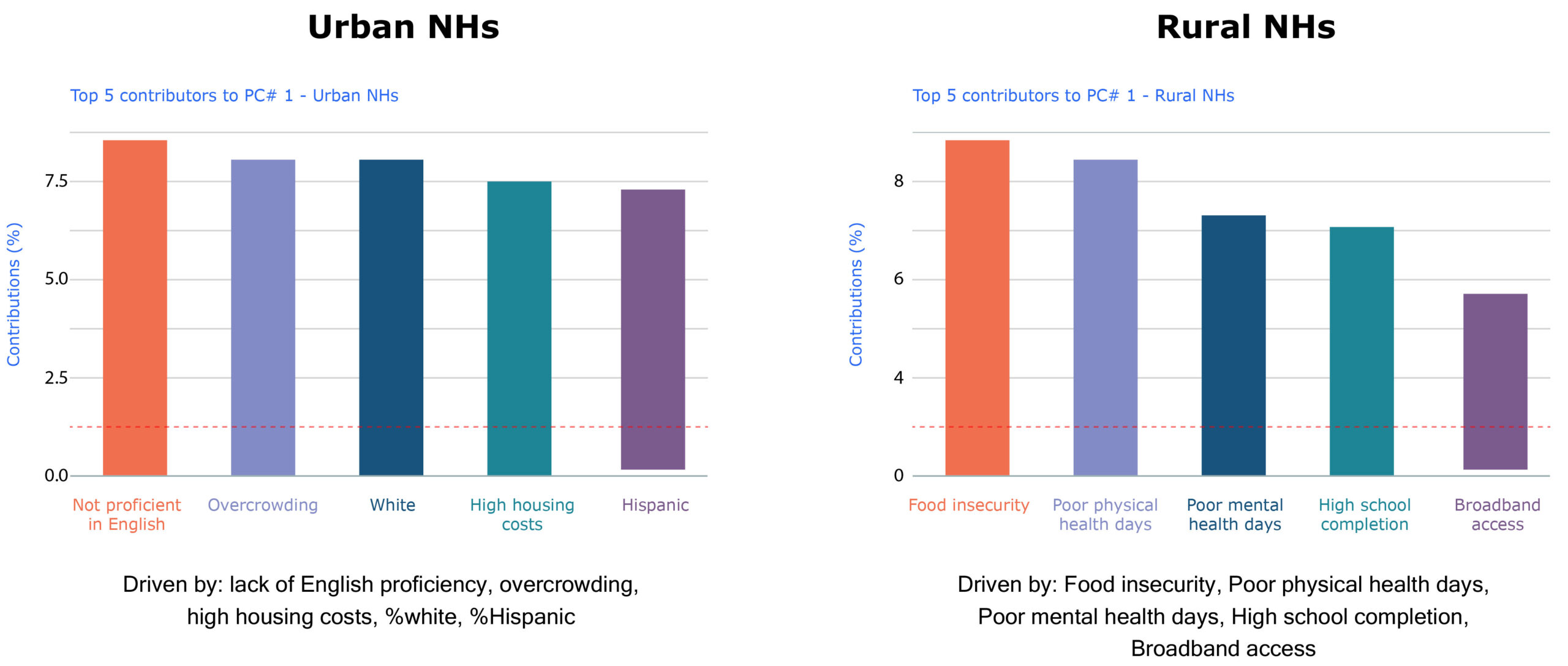
Similarly, looking at one of the Nursing Home-focused principal components, the contributing factors are distinct for urban and rural Nursing Homes. The number of beds, occupancy level, total COVID-19 cases among staff and residents contributed to 10% of the variance among urban Nursing Homes while resident case counts and shortages of clinical staff, general staff, nursing staff, and aides contributed to 8% of the variance among rural Nursing Homes.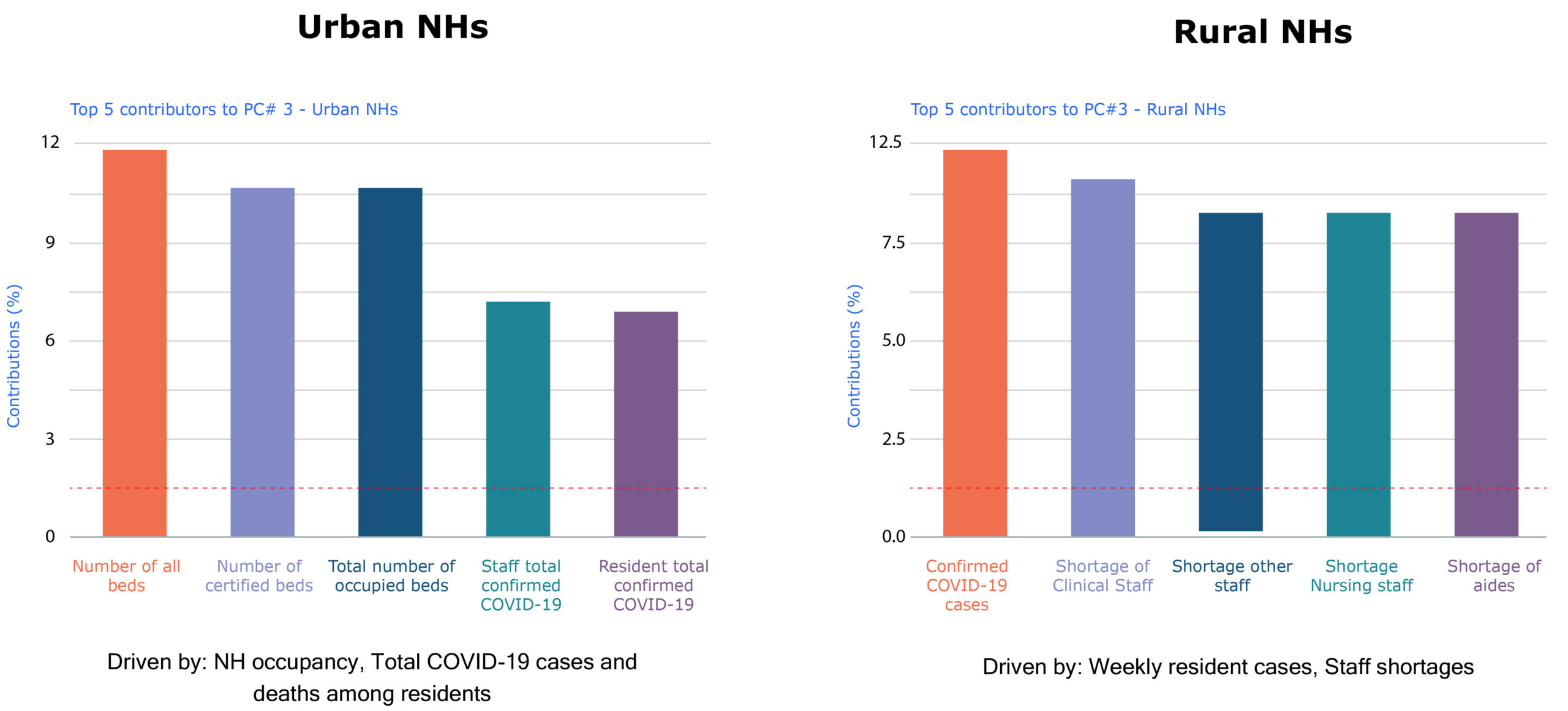
There are some important limitations of this analysis. Due to missing county-level health metrics, only 57.6% of the 15,272 Nursing Homes were represented. Moreover, this analysis was based on a strong assumption that county-level information was generalizable to Nursing Home Staff within a given county. Additionally, the use of PCA itself is limited to detecting linear relationships between variables. Therefore, there may be other SDOH factors not considered here that could be equally or more important.
Takeaways: Despite these limitations, this analysis offers a promising start to understanding and ultimately addressing vaccination from a SDOH lens, which is crucial because Nursing Home Staff are among the most socially vulnerable groups at risk of contracting COVID-19. They face a double whammy of risk inside and outside the workplace. As front-line caregivers to patients with compromised immune systems and multiple health complications, Nursing Home Staff are at increased risk of contracting COVID-19 through work, with a staggering mortality (2 deaths/1000 workers). Additionally, Nursing Home Staff, the majority of whom are Nursing Assistants, are often disadvantaged; more than 90% are women, 49% Black or Hispanic, 44% live in low-income households, and 36% are uninsured or on public health insurance — groups least likely to have access to community-testing due to social and economic factors stemming from long-standing structural racism.
Two years have passed and COVID-19 remains an ongoing challenge for the healthcare system. Vaccination is essential to protect Nursing Home Staff and ensure stability within the healthcare system. Staff shortages during the pandemic have disproportionately affected Nursing Homes, impacting the health, safety, and quality of life of residents and workers.
Innovation